Phase I results of UofL Health's Co-Immunity Project show precautions work to prevent spread of coronavirus
October 2, 2024Results from the first phase of the University of Louisville’s groundbreaking project to track COVID-19 in Metro Louisville show that precautionary measures to prevent transmission worked in preventing the disease’s transmission among health care workers.
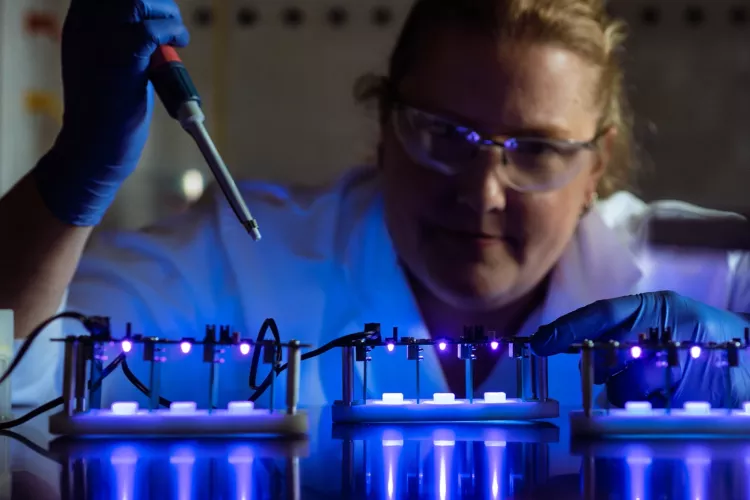
Throughout May, Phase I of the Co-Immunity Project tested 1,372 health care workers at hospitals in the UofL Health system. Samples were collected by UofL’s Christina Lee Brown Envirome Institute and tested at UofL’s Regional Biocontainment Laboratory at the Center for Predictive Medicine for Biodefense and Emerging Infectious Diseases.
The study found just two participants had an active infection of SARS-CoV-2, the virus that causes COVID-19. An additional 14 workers tested positive for antibodies, suggesting that they have been exposed to the virus. Unfortunately, due to low amounts of blood in some samples, antibody levels could not be tested in 128 workers.
The Co-Immunity Project, launched in April with an announcement by Kentucky Gov. Andy Beshear, is a collaboration between the Louisville Healthcare CEO Council and the Brown Envirome Institute. The purpose of Phase I of the project was to test health care workers at the Baptist Health, Norton Healthcare and UofL Health systems to identify those who have been exposed to COVID-19 and to determine how their body produced a response, or antibodies, to such infection. This information will help identify potential donors of high-quality plasma for treatment of patients with severe COVID-19 symptoms.
Interested health care workers collected their own blood and plasma samples and delivered them to researchers with the Brown Envirome Institute. The samples were then tested at the RBL, one of only 12 such NIH-funded laboratories in the nation and the only one in Kentucky. Results from Baptist Health and Norton Healthcare will be provided at a later date, but researchers say the results from workers at UofL Health facilities provide data that can be used to provide information about the pandemic and its effects.
UofL Health consists of five hospitals, four medical centers, nearly 250 physician practice locations, the UofL Health - Frazier Rehab Center and the UofL Health - James Graham Brown Cancer Center.
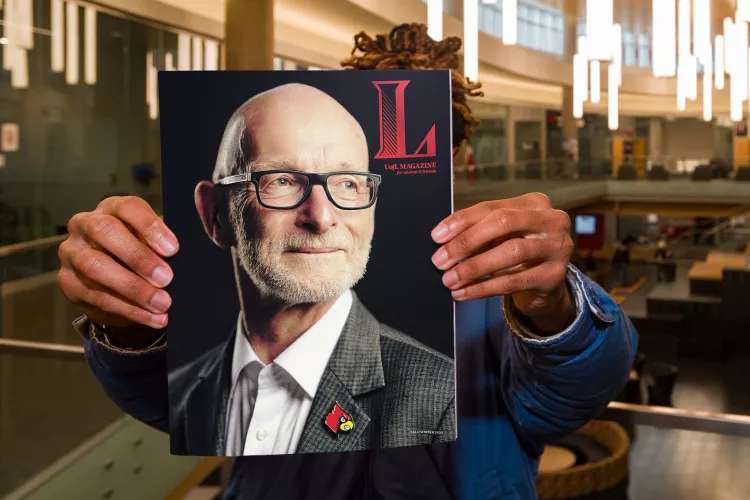
“The rates of infection and exposure among our health care workers is surprisingly low,” said CPM/RBL Director Kenneth Palmer, a co-investigator of the project. “Even though the number of individuals who tested positive for the antibody is more than those who had the active virus, this is still a low number, especially for those who are working in high-risk environments such as hospitals.”
“This is good news,” said UofL Assistant Professor of Medicine Rachel Keith, who conducted the study, “It shows that the precautionary measures adopted by our hospitals are working, and that patients seeking care in our hospitals are at a low risk of being infected by their health care providers.
“These results show the need for appropriate precautions, indicating that with proper PPE and social distancing, we can minimize the threat posed by the virus to our health care community.”
Researchers advised, however, that because so little is known about the novel coronavirus SARS-CoV-2 and the disease it causes, COVID-19, much more research is necessary.
“The rates of infection among health care workers nationwide remains unknown. A recent study of health care workers in Germany who had direct contact with COVID-19 patients did find that only 1.6% tested positive for SARS-CoV-2 antibodies. This is within range of the 1% of antibody-positive health care workers our study found in Louisville,” said Brown Envirome Institute Director Aruni Bhatnagar, a co-investigator with the project.
“However, fewer individuals with antibodies against the virus also could mean that few individuals have acquired immunity, and therefore many of our health care workers may be vulnerable to the virus still lingering in our community. They may remain susceptible should infections increase again, either in the fall or some other time.”
Individuals who have recovered from COVID-19 and have antibodies against the virus are being asked by Norton Healthcare to donate plasma to help treat high-risk patients. More information is available on the Norton Healthcare website.
Phase II of the Co-Immunity Project opened earlier this month to the community to sample 2,400 participants who reside in different parts of Jefferson County to determine the existing prevalence of COVID-19 infection and immunity in the general population.
The project also will re-test health care workers across UofL Health in July to see whether the rates of infection and immunity have changed since May. The results from this second survey will be critical in monitoring how an increase in non-critical care activities in UofL hospitals has affected SARS-CoV-2 infections and see what changes occur to the levels of antibodies in those who showed a positive antibody response in Phase I testing.