UofL lab helps discover new disease that causes kidney failure
October 2, 2024Researchers at the University of Louisville were part of a group that discovered an insidious new autoimmune disease that causes kidney failure.
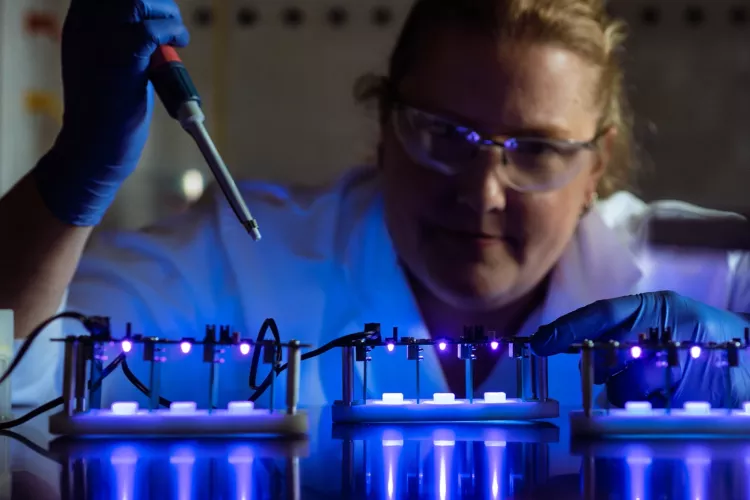
The discovery of anti-brush border antibody (ABBA) disease was made in the UofL Core Proteomics Laboratory, led by Director Jon B. Klein, MD, PhD, UofL School of Medicine vice dean for research and professor of medicine, and James Graham Brown Foundation Chair in Proteomics. Klein worked with the laboratory’s Co-Director Michael Merchant, PhD, associate professor in the Division of Nephrology & Hypertension in the Department of Medicine at UofL.
Klein and co-investigators presented their findings Nov. 3 at the American Society of Nephrology’s annual meeting in New Orleans.
“It’s the first time in my career that I’ve described a new disease, and truthfully, most people in their career don’t stumble on this,” said Klein, who is internationally recognized for his expertise in biomarker discovery related to kidney disease and practices with UofL Physicians-Kidney Disease Program. “We don’t know yet whether this causes kidney failure in a lot of people. It’s early in the story.”
The UofL lab identified ABBA after analyzing biopsied kidney tissue from 10 patients who had developed acute kidney injury, a sudden episode of kidney failure or damage that happens within a few hours or days. The condition causes a build-up of waste products in the blood and makes it difficult for kidneys to maintain adequate balance of fluid in the body.
For the first time, researchers discovered that in the nephrons, the functional units of the kidneys, antibodies had coated a specialized part of cells called brush borders, which help reabsorb and process proteins.
“The disease is rather insidious,” Klein said. “It was documented in a group of older men who simply turned up with abnormal kidney function, and there were no symptoms until they had very advanced kidney failure.”
Since it is an autoimmune disease, different approaches to suppress the immune system were used to treat the patients, but those efforts were unsuccessful, Klein said.
Further research will focus on defining demographics of patients with ABBA and the disease’s prevalence. Also, determining where on the protein megalin – which acts as a sponge to absorb proteins and other compounds that enter the nephron – the antibody binds is key to treating the disease, Klein said.
It’s unknown what stimulates the antibody formation.
“Antibodies have very specific targets; they bind to only certain proteins in autoimmune kidney diseases, and then to only certain portions of that protein,” Klein said. “That’s where you learn how to begin to block the antibody binding.”
Klein said the disease had gone undetected because most people with abrupt kidney failure recover and do not get biopsies. In cases of ABBA, however, kidneys do not improve.
Lead investigators of the study are Laurence H. Beck, MD, PhD, of Boston University School of Medicine, and Christopher P. Larsen, MD, a nephropathologist at Arkana Laboratories in Little Rock, Arkansas.
Related News